Under a new rule the Biden administration proposed on Tuesday, millions of Americans with obesity would be eligible to have popular weight-loss drugs like Wegovy or Zepbound covered by Medicare or Medicaid. The rule would not be finalized until January, days after President-elect Trump takes office.
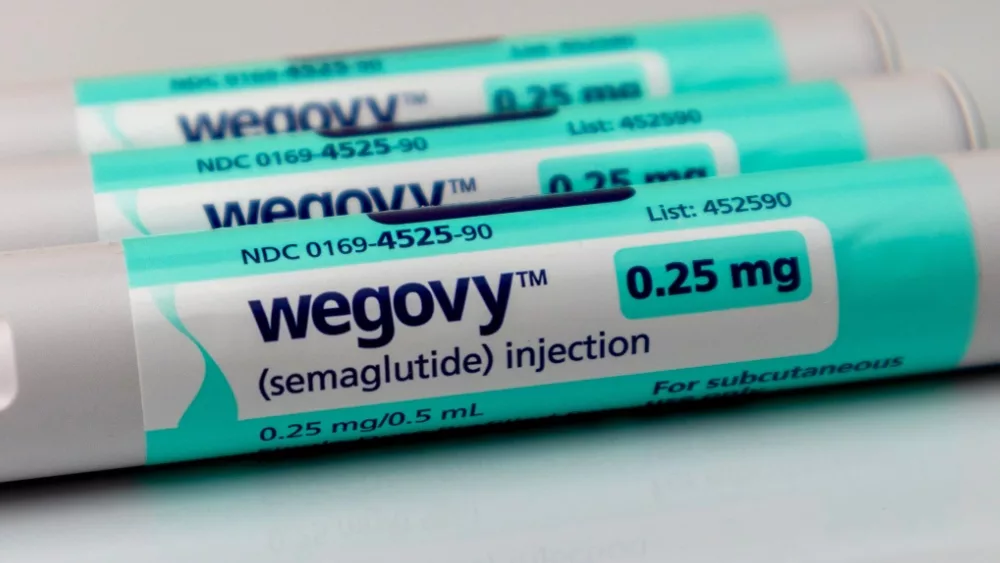
The new rule would dramatically expand access to anti-obesity medications such as Ozempic and Wegovy, from Novo Nordisk, and Mounjaro and Zepbound, from Eli Lilly. The White House said in a fact sheet that some 3.4 million Medicare beneficiaries and about 4 million Medicaid recipients would gain access to these medications, which can cost as much as $1,000 a month for the uninsured. Some Medicare enrollees could see their out-of-pocket costs drop by as much as 95%.
The Biden administration said: “This proposal would allow Americans and their doctors to determine the best path forward so they can lead healthier lives, without worrying about their ability to cover these drugs out-of-pocket, and ultimately reduce health care costs to our nation.”
Currently, Medicare has been barred from paying for weight loss drugs unless they’re used to treat conditions like diabetes or to manage an increased risk of heart disease. The Biden administration is proposing to reinterpret the law barring coverage by classifying obesity drugs as treatment for a “chronic disease,” rather than as weight loss medications. Centers for Medicare and Medicaid Services Administrator Chiquita Brooks-LaSure said on a call with reporters Tuesday: “The medical community today agrees that obesity is a chronic disease. These drugs are the beginning of a revolution in the way that weight is controlled.”
U.S. Health and Human Services Secretary Xavier Becerra told The Associated Press: “It’s a good day for anyone who suffers from obesity. It’s a game changer for Americans who can’t afford these drugs otherwise.”
Editorial credit: KK Stock / Shutterstock.com